Vavlukis, Marija and Caparovska, Emilija and Pocesta, Bekim and Kotlar, Irina and Kitanoski, Darko and Shehu, Enes and Taravari, Hajber and Bojovski, Ivica and Risteski, Dejan and Kedev, Sasko (2015) Predictors of in-hospital mortality in patients with acute or acute worsening chronic heart failure. In: Congress: Acute Cardiac Care 2015, 17-19 Oct 2015, Vienna, Austria.
![poster [thumbnail of poster]](https://eprints.ugd.edu.mk/14324/1.hassmallThumbnailVersion/Predictors%20of%20in-hospital%20mortality%20in%20patients%20with%20acute%20or%20acute%20worsening%20chronic%20heart%20failure.jpg)
Predictors of in-hospital mortality in patients with acute or acute worsening chronic heart failure.jpg
Download (608kB) | Preview
Predictors of in-hospital mortality in patients with acute or acute worsening chronic heart failure.pdf
Download (612kB) | Preview
Abstract
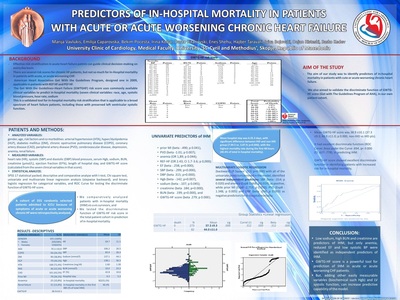
Aim of the study: to identify predictors of in-hospital mortality in acute HF patients. Patients and methods: 355 randomly selected patients admitted to ICCU with symptoms of HF were analyzed for: risk factors and co-morbidities (COPD, CAD, PVD, anemia, renal failure), heart rate, systolic and diastolic BP, Hgb, sodium, BUN, creatinine, ejection fraction (based on which patients were divided in PEF-HF and REF-HF); length of stay and GWTG-HF score (Get with the Guidelines-HF risk score), calculated from the seven clinical variables in that score. Comparative analyze was performed between patients with in-hospital mortality (IHM) and survivors. Statistical analyze: univariate and multivariate binary and linear logistic regression, ROC Curve for testing of discriminate function of GWTG-HF score. Results: 355 patients at mean age 70.1±10.9, 150 (42%) females and 205 (58%) males were included. Females were older 72.9±11.4 vs. 67.9±10.0 (p=0.000), had higher DBP (p 0.007) and EF (%): 43.6±11.6 vs 41.1±9.5 (p 0.029), and sodium level (p 0.018), more often had HTA (OR 1.4; p=0.001), while males had PAD (OR 1.7; p 0.020), and prior MI (OR 2.2; p 0.001). No significant differences in death rate, length of hospital stay and GWTG-HF score was observed. 82 (23.1%) events were registered (IHD group). The highest mortality rate was observed during the first 48 hours (40.4%). Mean hospital stay was 6.3±5.3 days, with no differences between the groups (5.6±3.9 vs. 6.7±5.9; p=0.056). We identified several univariate predictors: prior MI (beta -.490; p 0.041), PVD (beta -1.01; p 0.007); anemia (OR 1,89; p 0.044); REF-HF (OR 2.43; CI 1.7-3.6; p 0,000); EF (beta -.258; p=0.000); SBP (beta -.299; p=0.000), DBP (beta .315; p=0.000); Hgb (beta -.142; p=0.007), sodium (beta -.107; p 0.045); creatinine (beta .184; p=0.000), BUN (beta .199; p=0.000), and GWTG-HF score (beta .279; p 0.000). Multivariate logistic regression identified SBP (beta -.014; p 0.020) and anemia (ExpB 3.668; p 0.019); as positive, while prior MI (ExpB -2.753; p 0.050); PVD (ExpB -1.348; p 0.005) and DBP (beta .034; p 0.003) as negative predictors for in-hospital death. Mean GWTG-HF score was 38.9 ±10.1 (37.3 ±9.3; 44.0 ±11.0; p 0.000, non-IHD vs IHD pts). It had excellent discriminate function (ROC Curve: Area under the Curve .694, p< 0.000 (CI .627-.778), in predicting IHD. Conclusion: Low sodium, high BUN and creatinine are predictors of IHD, but only anemia, reduced EF and low systolic BP were identified as independent predictors of IHD. GWTG-HF score is a powerful tool for prediction of IHD in acute or acute worsening CHF patients.
| Item Type: | Conference or Workshop Item (Paper) |
|---|---|
| Subjects: | Medical and Health Sciences > Clinical medicine |
| Divisions: | Faculty of Medical Science |
| Depositing User: | Marija Vavlukis |
| Date Deposited: | 16 Dec 2016 11:21 |
| Last Modified: | 16 Dec 2016 11:21 |
| URI: | https://eprints.ugd.edu.mk/id/eprint/14324 |
